Cumbria Strategy for Digital Technologies in Health and Social Care
TWO KEY QUESTIONS:
- What do we mean by good health and social care in a rural setting?
- How can digital technologies address some of the issues?
1. Introduction
The University of Cumbria was commissioned to work with the Cumbria Rural Health Forum to develop the Cumbria Strategy for Digital Technologies in Health and Social Care. The work was carried out from 1st April 2014 to 30th June 2015 and was funded by the Academic Health Science Network for North East and North Cumbria (AHSN-NENC). An implementation phase followed, from 1st July 2015 to 31st March 2016, funded jointly by the Academic Health Science Network for North East and North Cumbria and the North West Coast Academic Health Science Network (NWC AHSN).
The Strategy was developed through a range of methods, including review of published literature and evidence, surveys and interviews and open innovation roadmapping workshops. The implementation phase focused on supporting, facilitating and influencing change, through engagement with providers and service delivery staff and presentations to senior managers.
The outcome of this work was to embed the work of the Forum in the Local Digital Roadmap and Sustainable Transformation Plans for NHS partners, to support third sector and private sector partners and to share best practice nationally and internationally.
Further reading:
2. What do we mean by digital technologies in care?
In this document, the term ‘digital health’ is defined broadly to include the use of information and communications technologies to replace, augment or complement conventional face to face health and social care delivery.
We include telehealth, telemedicine, telecoaching, telecare, assistive technologies, e-health, mobile apps and wearable telemonitoring. The focus of the discussion has always been on mature, commercially available products and services, seeking to share best practice and understand the benefits and barriers to adoption.
The project excluded services that are used primarily in administrative functions, such as the use of email or SMS messaging for appointment reminders, to focus on those that affect health and care professionals in the delivery of care.
3. What are the specific issues for care in rural communities?
Identified issues for rural health and social care in Cumbria
- Dispersed communities meaning that people have limited access to services and have to travel further to access basic healthcare
- Smaller GP practices and other health centres, meaning that staff may feel professionally isolated and removed from opportunities for professional development
- A greater reliance on volunteer services
- Population demographics that include relatively more older people than in urban centres
- Poor quality broadband and mobile infrastructure
Further reading:
- Brief on connectivity
- Report on learning from international projects using digital health in rural areas
Note on terminology
Whilst much of Cumbria does not meet the approved DEFRA definition of rural (outside of a settlement of 10,000 or more residents), it was agreed that the whole of Cumbria is affected by rural issues because of the distances of travel between the larger settlements and the fact that there is no large conurbation within the county. A more correct term may be ‘dispersed’ or ‘hard to reach’ populations, but comparison with use of terminology elsewhere suggests that ‘rural’ is widely acceptable.
4. What is already being done in Cumbria or elsewhere?
We carried out a mapping project to find out what existing digital health and care projects were happening in or adjacent to Cumbria, between July 2014 and May 2015. Forum members were asked to advise us of projects that are either being piloted, ready for roll out or had been piloted and not adopted. In total 27 projects were identified and a full listing can be provided on request. Two successful projects that are in service use are described below.
- Out of hours stroke assessment and consultation: NCUHT with NW Shared Infrastructure Services. Since July 2012 – over 400 patients have used the service
- www.patientmemoirs.com A platform for patients, carers and others to maintain video logs of their reflections, learn from their experiences, share tips and ideas.
Further reading:
5. Identify needs and opportunities for digital technologies in care within Cumbria
Two separate qualitative studies were undertaken with a) long term conditions patients b) rural GPs
- How could you use technology in managing your/your patients’ healthcare?
- What is possible now? What would you like to be possible?
- What are the barriers?
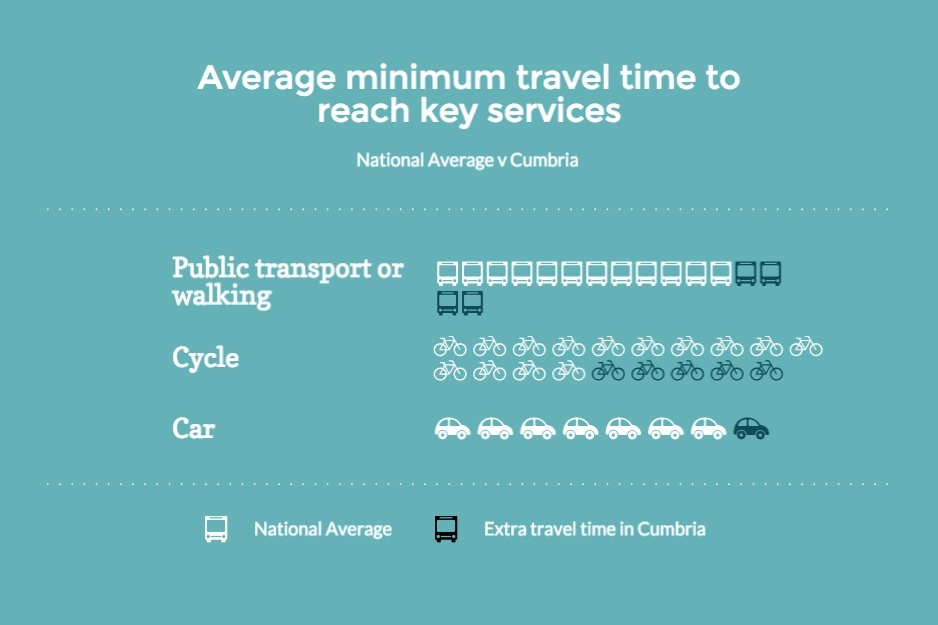
The Cumbria Joint Strategic Needs Assessment highlights the issue of accessibility. The average minimum travel time to reach key local services (including GPs and hospitals) across Cumbria was 16 minutes by public transport / walking, 14 minutes by cycle and 7 minutes by car; these times were all longer than the national averages of 12, 9 and 6 minutes respectively.
A Round Table discussion with representatives of key providers, commissioners, representatives of third sector services was held in June 2015. Work to share and combine strategies for digital health in Cumbria is being undertaken.
Further reading:
- Brief on GP Perceptions of Technology Study
- Brief on Long Term Conditions Patients’ Perceptions of Technology Study
- Brief on Working with the Third Sector
- Video of Rheged Technology Enabled Care in Cumbria Event (June 2015)
6. A roadmap for implementation of digital health and social care in Cumbria
Three key themes were identified from the strategy and were implemented through a range of activities and events. Click on the links below to access detailed information on each theme.
| Objective | Activity | Who is involved | Next steps |
|---|---|---|---|
| Improve health outcomes for those with long term conditions. Support more to self manage | Cumbria-wide co-ordinated implementation of digital health and care, for specific services | CCG GPs NHS Trusts CCC Third sector Private sector |
'Digital think tanks' workshops with services, departments, GP practices |
| Implementation - facilitating service change | |||
| Explain, clarify, share good (and bad) practice, assess impact and value | Information exchange, portal for what good rural health looks like, sharing experiences and equipment, conferences and events, influencing and advocacy for Cumbria | All partners and associates | Extend, enhance maintain website Networking events Conferences Briefing papers and ‘how to’ guidance Influencing policy in partner organisations |
| Implementation - sharing best practice and value | |||
| Develop a digital-healthready workforce | Training and professional development to support health professionals to use digital health and enhance the ‘Cumbrian offer’ for recruitment and retention | CLIC UoC Solution providers – private sector Third sector |
Training and networking events with CPD groups Materials and programmes NHS England Code4Health community |
| Implementation - creating a digital-health-ready workforce | |||
7. Authors and Acknowledgements
The Cumbria Rural Health Forum has received funding from the Academic Health Science Network for North East and North Cumbria (AHSN NENC) and the North West Coast Academic Health Science Network (NWC AHSN).
The project is managed by the University of Cumbria. The website is hosted by the Cumbria Partnership NHS Foundation Trust. The project steering group are:
- Alison Marshall (University of Cumbria)
- Tom Bell (Cumbria Partnership NHS Foundation Trust)
- John Roebuck (Cumbria Clinical Commissioning Group)
- Lorraine Smyth (Action for Communities in Cumbria)
- Peter Knock (Cumbria County Council)
In kind support from these organisations and from all the partner organisations has included provision of meeting rooms, catering, printing, management time. A full list of Forum partners is available at http://www.ruralhealthlink.co.uk/about-us/partners/
This report includes contributions from Jae-Llane Ditchburn, Tom Bell, Lorraine Smyth, Keith Jackson, Frank Peck, Alan Lillie, Peter Knock. The report was edited by Alison Marshall to whom any comments or feedback should be addressed at alison.marshall@cumbria.ac.uk